 [1] [1] | |
| Drug Name | Valproate |
|---|---|
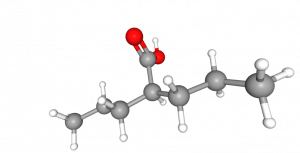
| Systematic name | 2‐propyl‐pentanoic acid |
| Type | Anti-epileptic drug (AED) |
| Molecular formula | C8H16O2[1] |
| Molecular weight | 144.21 g/mol[1] |
Contents
General
Valproate (VPA) is a drug used in the treatment of epilepsy, bipolar disorder and spinal muscular atrophy [2] . VPA is used to control epileptic seizures, divided in two subcategories: focal and generalized seizures.
VPA was originally synthesized by Burton in 1882 and used as an organic solvent. Its antiepileptic effect was discovered by accident almost 100 years later by Meunier et al. (1963). It was registered as a drug in 1964 in France and later in many other countries. [3][4][5]
Structure and interaction with albumin
VPA (2‐propyl‐pentanoic acid) is a short-chain fatty acid ingested intravenously or orally as sodium valproate, composed of sodium and VPA in a 1:1 molar ratio. VPA itself is highly hydrophobic, leading to a favourable entry to the central nervous system with good oral bioavailability. [6] VPA in the blood exists in its free form as the valproate ion, but is highly bound to serum proteins. It mainly binds to albumin (90 - 95%), [7] with the unbound fraction increasing linearly from approximately 10% at 50 mg/L to approximately 30% at 200 mg/L total concentrations. [6] Phenytoin, another well-known anti-epileptic drug (AED), is a competitor in this protein binding. This means that VPA binding to albumin decreases if phenytoin is taken, causing both free drug concentrations to increase. [8]
Mechanism of action
Pathophysiology of epilepsy
Epilepsy is a disease of the central nervous system caused by disruptions in the electrical communication between neurons, more specifically, the imbalance in excitatory and inhibitory action of neurotransmitters at the synapses, which can lead to seizures, loss of awareness or unusual behavior. [9] A seizure occurs when there is a large depolarization of many neurons that fire the action potential at the same time. This paroxysmal depolarizing shift can last for thirty seconds up to two minutes and leads the above mentioned effects. The focal seizure starts in one part of the brain, but due to the failure of inhibitory mechanisms it can spread further. The cause of it can be a trauma or cortex developmental disorder [10] [11] The generalized seizure, on the other hand, is characterized by a sudden and large activity that occurs in more than one area of the brain at the same time, causing the hyperexcitability in the cortex and the neurons that connect the thalamus to the cortex. [12]
Genetic Pathophysiology
One of the reasons for epilepsy development is the genetic background. While the exact background is still unknown, there are certain genes that were found to be involved in the progression of the epilepsy, for example SCN1A and SCN8A that are active in the production of sodium channels and can therefore contribute to the epilepsy succession. [13] Epilepsy is split into two types: focal and generalized. The first type of focal seizures is the one without loss of consciousness, but with jerking of different body parts or a change in the perception of reality. The second type is focal seizures with impaired consciousness or change of awareness. On the other hand, generalized epilepsy types are absence seizures, tonic seizures, atonic seizures, clonic seizures and so on. [14] Focal seizures include automatisms, behavior arrest, hyperkinetic, autonomic, cognitive and emotional, while atonic, clonic, epileptic spasms, myoclonic and tonic seizures can be both focal or generalized. Generalized seizure types absence with eyelid myoclonida, myoclonic absence, myoclonic - atonic, myoclonic - tonic - clonic. [15]
Valproate Mode of Action
The exact mode of action of valproate on molecular level is unknown, as there are many different substances that participate simultaneously in the regulation of neuronal activity. [2] VPA is connected to cortical inhibition in order to contribute to ‘neural synchrony’ and is known to provide protection from neural degradation and damage. [16] VPA inhibits histone deacetylase, which causes hyperacetylation of histones. The drug is furthermore connected to inositol depletion by preventing the gene prolyl oligopeptidase to be expressed through indirect inhibition of myo-inositoal-1-phophate-synthetase. [16] In terms of epilepsy, it is believed that VPA is affecting the activity of GABA. By increasing the activity of GABA, the epileptic attacks are prevented. This is established through inhibition of succinic semialdehyde dehydrogenase which then increases the amount of succinic semialdehyde and subsequently increases GABA neurotransmission. [17]
VPA affects the extracellular signal-regulated kinase pathway or ERK (Extracellular Receptor Kinase), which results in phosphorylation of ERK 1/2 . This has an effect on the expression of proteins that contribute to the plasticity of neurons and neuronal growth. The downside of this effect of VPA is the additional increase in GABA activity. VPA has an influence on fatty acids production, leading to lower membrane fluidity due to the presence of less sterols and glycerolipids. Subsequently, this increases the action potential threshold of the membrane and contributes to the antiepileptic effects of valproate . [18]
Pharmacokinetics of VPA
When introduced orally, VPA is found to be absorbed in a period of 4 hours. However, introducing it in other ways results in the same Cmax, AUC and Cmin in a steady state, while all the differences in absorption are neglected. When VPA is taken as extended release tablet and combined with meals, the absorption time increases from 4 to 8 hours. On the other hand, the increase in absorption time in the same situation increases from 3.3 to 4.8 hours when taken as a sprinkle tablet. There is 90% bioavailability of VPA in all oral forms. On the other hand, there is 100% bioavailability in enteric-coated forms. [19]The average half-life of VPA is 13-19 hours, the volume of distribution is 11 L/1.73 m2 . The protein binding is linear at low concentrations, but non-linear and decreased at high concentrations, which may be due to the different affinity binding sites of albumin. Parts of the drug can be metabolized in different ways. The most relevant metabolism of VPA would be glucuronide conjugates and mitochodrial-ß oxidation. [18]
Only 3% of the drug is eliminated through urine, about 30-50% is eliminated through hepatic metabolism, as well as about 40% being excreted through mitochondrial-beta oxidation. [19]
Efficacy and influence on hepatic function
Optimal dose and effects are achieved with upper limit of 60 mg/kg/day. If the desired effects are not achieved (in other words, the seizures are not gone or the side effects are too strong), testing for blood levels of VPA needs to be executed in order to determine whether they fall within the optimal range of total VPA 50-100 µg/mL. Otherwise, the dose is altered in agreement with the doctor according to the individual state of the patient, his/her other conditions or other medication that they take. The toxicity level of valproate in blood, although not very conclusive, is taken as 150 µg/mL[20] .
VPA impacts the hepatic drug metabolism by inhibiting it and displacing other strongly bound drugs from proteins, which implies that dosage changes need to be considered when using it in combination with other drugs. [21] The normal limits of valproate in blood of 70-100 kg person is 1000-3000 mg/day [22]
Number of patients
Epilepsy affects around 50 million people worldwide. This includes people having less than one seizure per year. The prevalence of active epilepsy (i.e. patients who have frequent seizures or use medication) is between 0.4% and 1%. On a global scale, an estimated five million people are diagnosed with epilepsy each year. Epileptic seizures can be controlled by using anti-epileptic drugs (AEDs). About 70% of epileptic patients becomes free of seizures by appropriate AEDs. Low-cost treatments are available, with daily medication that costs as little as US$ 5 per year.[23]
Medical use and TDM
Valproate (VPA) is usually taken as tablets of 250 mg or as a syrup with 250 mg per ml, but this may vary per product [24].The dose of VPA is at first taken in small amounts and is then gradually increased until the satisfactory dose is reached. Testing for valproate levels is important to check if the blood levels are within normal therapeutic range [21] . The test should measure the free concentration (i.e. the concentration of unbound valproate) as this fraction is pharmacologically active. The recommended levels of unbound valproate are 6-22 µg/mL in blood [21].For epilepsy patients, the range for the treatment of total valproate should be 50-100 µg/mL. Overall, if a patient has a VPA concentration that falls within this range, does not have recurrent seizures and has minimal side effects, then the dose is said to be suitable[21] . To provide a patient their right amount of medication, therapeutic drug monitoring (TDM) is implemented in hospitals, because every patient responds differently to a certain dose of medication. VPA is a conventional drug that is used as first line monotherapy for idiopathic generalized epilepsies. Its effectiveness is not clearly conclusive and varies between different patients. The doses are not generalized and depend on patient’s age and weight. Doses are taken every day, with some patients even two times a day. It is not advised, but sometimes necessary, to take VPA in combination with other seizure drugs (e.g., ethosuximide, lamotrigine, phenytoin, rufinamide, topira mate), some antidepressants or certain antibiotics[21] Medications based on VPA are harmful for the unborn child. If valproate is taken during pregnancy, research has shown that up to 4 in 10 babies are at risk of developmental disorders, and approximately 1 in 10 are at risk of birth defects. [25]
Safety & Lab protocols
Safety
All anti-epileptic drugs have side-effects, including VPA. The risk of hyperammonemia is nearly 40% in patients ingesting intravenous VPA in the ICU setting [26] . Other adverse effects include thrombocytopenia and endocrine effects of women. Valproate is associated with a dose-related teratogenicity rate, with risk of major malformation higher than 30% at doses greater than 1100 mg/d. In utero exposure is also linked to dose-dependent reduced verbal IQ and autism[27] . Children, who were exposed to VPA during birth, have a possible chance of a major congenital malformation (MCM) [28] . The risk of having severe consequences for these infants exposed to sodium valproate in utero has been estimated between 6% and 12%[29] . This can be prevented by reducing the dose of the drug. An example of endocrine effects might be idiosyncratic liver toxicity [30]
Lab Protocols
VPA is considered thermodynamically stable, which indicates that it is not reactive under normal environmental conditions. It should be stored in a metal can or drum and kept away from incompatible materials such as oxidizing agents, bases and strong reducing agents as ignition may result.
Working with VPA can be irritating when inhaled or when getting directly in contact with the yes. To prevent this, VPA needs to be handled in a fume hood, safety goggles, lab coats, and gloves need to worn. Direct skin contact or ingestion of VPA should be avoided. In case of contact, flush the specific body part and go to the doctor without delay [31]
State of the art
| Company | Product | Test name | Sample Volume (μL) | Reportable range | Dilution | Precision | Incubation time | Measuring Technique |
|---|---|---|---|---|---|---|---|---|
| Beckman Coulter[32] [33] | AU2700/AU5400 | VALPROIC ACID EMIT® 2000 | 3.5 μL | < 150 μg/mL | 1:1 | Total CV < 4.3% Inter-assay: CV < 3.2% |
15-75 min. | ELISA1 |
| Roche COBAS[34] [35] | Cobas 8000 | Cobas 8000 | 1.5–35 | 3.15 – 150 mg/L [36] | 1:(3-121) | Inter-assay: CV < 0.7% ~ 2.9% Total CV<3% |
9 min – 27 min | ELISA1 |
| ABBOTT LABORATORIES DIAGNOSTIC DIVISION[37] | B1P350 | ARCHITECT iValproic Acid | 10 | 2 - 150 μg/mL | 1:10 | Total CV≤ 7% | 29 min | CMIA2 |
| SIEMENS HEALTHCARE DIAGNOSTICS INC.[39] | 67070 | ADVIA 1200 CHEMISTRYSYSTEM -VALPROIC ACID (VPA) ASSAY | 2-3 | NA | 1:5 | Inter-assay: CV = 0.2% - 5.3 % Total CV= 0.4%-5.3% [40] |
3-21 min | ELISA1 |
| MICROGENICS CORPORATION[41] | 62390 | CEDIA TDM ASSAY -VALPROIC ACID | NA | 3.0-150 μg/mL | NA | Inter-assay: CV = 1.3% - 2.4 % Total CV= 1.8%-3.4% |
Reagent 1 : 2-5 min Reagent 2: 4-8 min |
ELISA1 |
Note: 2.CMIA: Chemiluminescent Microparticle Immunoassay
To measure unbound VPA, blood samples are treated by ultrafiltration, followed by an immunoassay, also referred to as ELISA. By performing the ultrafiltration, the bound form of VPA is separated from its unbound form. After that, the level of the unbound fraction can be measured by an immunoassay, e.g. an ELISA kit. Alternatively, LC-MS can be used to measure VPA.[42] In contrast to an HPLC assay, steps such as extraction, solvent or derivation must be executed prior to a HPLC assay, which takes significant more time[38] . CMIA is a special type of ELISA [43] . Several innovations are being investigated for VPA testing. For example, 2D-LC system (two-dimensional chromatography) was studied, allowing large volume injection, reducing interfering components, and reducing the analysis time and preventing most interference components by selecting useful sections in the “heart-cut” column(1D) from entering the analysis column (2D).[44] . Another example is dried blood spot (DBS) followed by gas chromatography mass spectrometry (GC–MS), which does not require solvent extraction or elution. The limit of quantitation was 200 ng/mL. [45]
References
- ↑ 1.0 1.1 1.2 Pubchem (Last modified: 2019-12-08) Accessed on 12 December 2019, at https://pubchem.ncbi.nlm.nih.gov/compound/Valproic-acid#section=3D-Conformer.
- ↑ 2.0 2.1 Sodium valproate (Epilim, Epival, Episenta). (2018, June 5) , at “https://www.netdoctor.co.uk/medicines/brain-nervous-system/a6665/epilim-sodium-valproate/”.
- ↑ , . Drugbank, Valproic Acid Retrieved from November 25, 2019, at [https://www.drugbank.ca/drugs/DB00313 “https://www.drugbank.ca/drugs/DB00313”].
- ↑ Perucca, E. (2012, August 29). Pharmacological and Therapeutic Properties of Valproate ,CNS Drugs October 2002, Volume 16, Issue 10, pp 695–714. Retrieved November 28, 2019, at “https://link.springer.com/article/10.2165/00023210-200216100-00004.”
- ↑ Padmanabhan, R., Abdulrazzaq, Y. M., & Bastaki, S. M. A. (2000). Valproic acid-induced congenital malformations: Clinical and experimental observations , Congenital anomalies 40(4), 259-268. Retrieved December 9, 2019, at [1].
- ↑ 6.0 6.1 Williams, J. H., Jayaraman, B., Swoboda, K. J., & Barrett, J. S. (2011, December 13). Population Pharmacokinetics of Valproic Acid in Pediatric Patients With Epilepsy: Considerations for Dosing Spinal Muscular Atrophy Patients. Retrieved October 17, 2019 , at “https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3345311/”.
- ↑ Dasgupta, A. (2016). Chapter 4 - Monitoring Free Drug Concentration: Clinical Usefulness and Analytical Challenges. Retrieved October 17, 2019 , at “https://doi.org/10.1016/B978-0-12-802025-8.00004-0”.
- ↑ Cramer, J. A., & Mattson, R. H. (1979). Valproic acid: in vitro plasma protein binding and interaction with phenytoin. Retrieved November 6, 2019 , at “https://www.ncbi.nlm.nih.gov/pubmed/121944”.
- ↑ Flyyn, S., & Babi, M. A. (2017). Pathophysiology of Epilepsy.Paragraph Anticonvulsants , at “https://www.sciencedirect.com/topics/medicine-and-dentistry/pathophysiology-of-epilepsy”.
- ↑ (Nall, R. R. (2018, January 23). What are simple partial seizures? Retrieved December 7, 2019, at [ https://www.medicalnewstoday.com/articles/320696.php“ https://www.medicalnewstoday.com/articles/320696.php”].
- ↑ (Leventer, R. J., Guerrini, R., & Dobyns, W. B. (2008, March 1). Malformations of cortical development and epilepsy. Retrieved December 7, 2019, at [2].
- ↑ (2016, May 22).2-Minute Neuroscience: Epilepsy. Retrieved November 26, 2019, at “https://www.youtube.com/watch?v=OGFQhLPaaOQ”.
- ↑ Guo, W., Shang, D.-M., Cao, J.-H., Feng, K., He, Y.-C., Jiang, Y., … Gao, Y.-F. (2017). Identifying and Analyzing Novel Epilepsy-Related Genes Using Random Walk with Restart Algorithm. Introduction , at “https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5309434/”.
- ↑ Epilepsy. (2019, August 10), at “https://www.mayoclinic.org/diseases-conditions/epilepsy/symptoms-causes/syc-20350093”.
- ↑ Fisher, R. S., Cross, J. H., French, J. A., Higurashi, N., Hirsch, E., Jansen, F. E., … Zuberi, S. M. (2017, April). Operational classification of seizure types by the International League Against Epilepsy: Position Paper of the ILAE Commission for Classification and Terminology, at [ https://www.ncbi.nlm.nih.gov/pubmed/28276060 “h https://www.ncbi.nlm.nih.gov/pubmed/28276060 ”].
- ↑ 16.0 16.1 Williams, R. S. B., Cheng, L., Mudge, A. W., & Harwood, A. J. (2002). A common mechanism of action for three mood-stabilizing drugs , at “https://www.nature.com/articles/417292a”.
- ↑ Flyyn, S., & Babi, M. A. (2017). Pathophysiology of Epilepsy , at “https://www.sciencedirect.com/topics/medicine-and-dentistry/pathophysiology-of-epilepsy”.
- ↑ 18.0 18.1 , . Drugbank, Valproic Acid Retrieved from November 25, 2019, at [https://www.drugbank.ca/drugs/DB00313 “https://www.drugbank.ca/drugs/DB00313”].
- ↑ 19.0 19.1 Gugler, R., & Unruh, G. E. von. (2012, December 13). Clinical Pharmacokinetics of Valproic Acid , at “https://link.springer.com/article/10.2165/00003088-198005010-00002”.
- ↑ valproic Acid Dosage Guide with Precautions. (2019, March 28), at “https://www.drugs.com/dosage/valproic-acid.html”.
- ↑ 21.0 21.1 21.2 21.3 21.4 Valproic Acid (2018, October 1) , at [3].
- ↑ Farmacotherapeutisch Kompas. Retrieved December 19, 2019, at [4].
- ↑ WHO. (2019, June 20). Epilepsy. Retrieved October 30, 2019 , at “https://www.who.int/news-room/fact-sheets/detail/epilepsy”.
- ↑ Valproic Acid Capsules - FDA prescribing information, side effects and uses. (2018, June 1).Retrieved November 26, 2019, at [5].
- ↑ gov.uk. (2018, March 23), at [6].
- ↑ Lind, J., & Nordlund, P. (2019, July). Intravenous use of valproic acid in status epilepticus is associated with high risk of hyperammonemia, Seizure Vol. 69. Retrieved October 23, 2019, at [7].
- ↑ Abou-Khalil, & Bassel, W. (2019). Update on Antiepileptic Drugs 2019. Retrieved November 6, 2019, at [ https://insights.ovid.com/crossref?an=00132979-201904000-00014“ https://insights.ovid.com/crossref?an=00132979-201904000-00014”].
- ↑ Morrow , J., Russell, A., Guthrie, E., Parsons, L., Robertson, I., Waddell, R., … Craig, J. (2006, January 17). Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. Retrieved October 23, 2019, at [8].
- ↑ Use of Sodium Valproate in Pregnancy. (2014, December 15). Retrieved October 23, 2019, at [9].
- ↑ Stewart, J. D., Horvath, R., Baruffini, E., Ferrero, I., Bulst, S., Watkins, P. B., … Chinnery, P. F. (2010, November). POLG determines the risk of sodium valproate induced liver toxicity. Retrieved October 23, 2019, at [10].
- ↑ Chemwatch: 15242 Version No: 7.1.1.1 Safety Data Sheet (Conforms to Regulation (EU) No 2015/830)
- ↑ Emit 2000 Valproic Acid Assay (2010, September) Retrieved from November 7, 2019. Beckman.
- ↑ Beckman Coulter system Reagent, AU400/AU400e (2012, February) Retrieved from November 7, 2019. Beckman.
- ↑ Cobas 8000 modular analyzer series (last update: 2019, November 8).
- ↑ van Eckardstein, A et al. (2013). cobas 8000 Modular Analyzer Series Evaluated under Routine-like Conditions at 14 Sites in Australia, Europe, and the United States. Retrieved from October 23., at [https://pdfs.semanticscholar.org/beb9/eaea6d45ba8fec2f3049cc5e242d9d2cfb13.pdf “https://pdfs.semanticscholar.org/beb9/eaea6d45ba8fec2f3049cc5e242d9d2cfb13.pdf ”].
- ↑ Therapeutic drug monitoring (2011). Retrieved from November 8, 2019. R-Biopharm AG.
- ↑ iValproic Acid B1P350 (2009,August).
- ↑ 38.0 38.1 Free Valproic Acid Assay (2014, April). Retrieved from November 3, 2019, at [11].
- ↑ ADVIA 1900 Chemistry system
- ↑ American Association for Clinical Chemistry, 70th AACC Annual Scientific Meeting (July, August, 2018). Retrieved from November 7, 2019
- ↑ CEDIA Valproic Acid II Assay (2018, November). Retrieved from November 7, 2019
- ↑ ao, S., Miao, H., Tao, X., Jiang, B., Xiao, Y., Cai, F., … Chen, W. (2011, July 1). LC–MS/MS method for simultaneous determination of valproic acid and major metabolites in human plasma, Journal of Chromatography B Volume 879, Retrieved November 28, 2019, at [12].
- ↑ Ilyas M., Ahmad. I (2014, July 12), Chemiluminescent microparticle immunoassay based detection and prevalence of HCV infection in district Peshawar Pakistan, third alinea Background, Retrieved from November 7, 2019, at [13].
- ↑ Liu, W., Shang, X., Yao, S., & Wang, F. (2019, August 20). A novel and nonderivatization method for the determination of valproic acid in human serum by two‐dimensional liquid chromatography. Retrieved October 17, 2019, at [14].
- ↑ Guo, M., Shao, L., Chen, X., Li, H., Wang, L., Pan, Y., & Tang, D. (2019, September 13). Assay of dried blood spot from finger prick for sodium valproate via ink auxiliary headspace gas chromatography mass spectrometry, Journal of Chromatography A Vol. 1601 p. 335-339. Retrieved October 24, 2019, at [ https://doi.org/10.1016/j.chroma.2019.05.039“ https://doi.org/10.1016/j.chroma.2019.05.039”].